Klebsiella pneumoniae virulence factor regulation in the respiratory tract
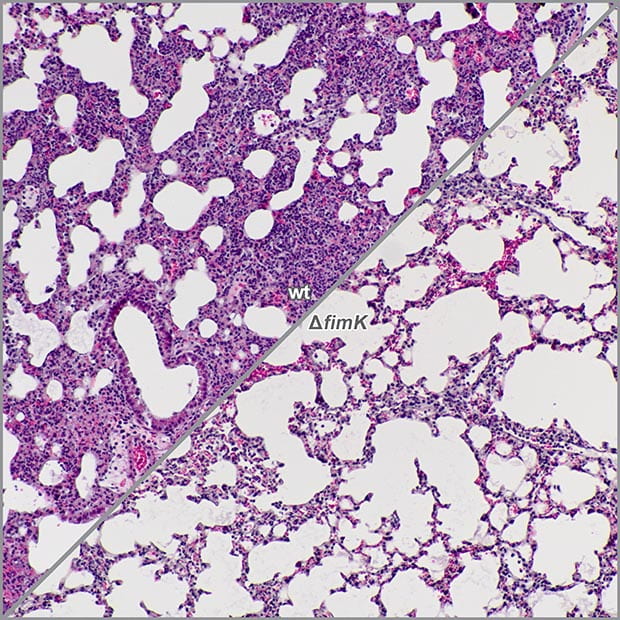
Klebsiella pneumoniae is one of the most common causes of nosocomial pneumonia and is difficult to treat given the high rate of antimicrobial resistance. We have developed mouse models of pneumonia that highly recapitulate human disease in order to study what factors are important for Klebsiella to survive in vivo. Capsule is known to be an important factor for virulence in the lung but its cues for expression are not well understood.
We have found that capsule expression may be counter-regulated by the expression of type 1 pili that may be important in other environmental niches outside the lung. Ongoing studies are aimed at uncovering the mechanisms Klebsiella uses to differentially express its wide range of virulence factors in response to host conditions and cues.
Adaptive immune responses to Klebsiella pneumoniae
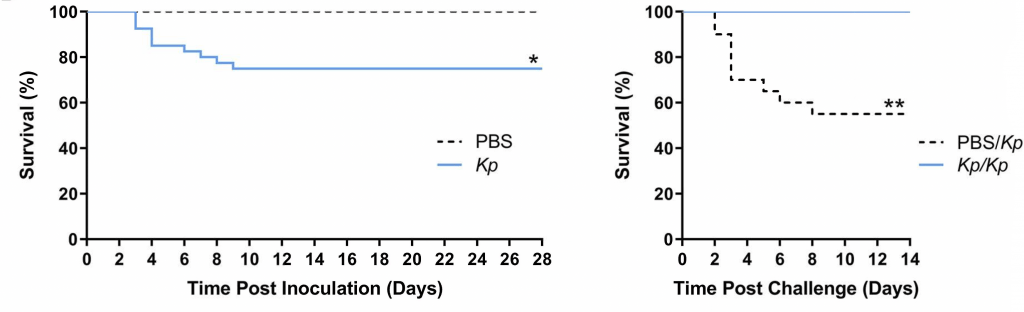
A vaccine to prevent Kp infections could potentially save the lives of many patients, particularly in light of the spread of highly antibiotic resistant strains. However, Kp can mask itself in one of eighty plus different polysaccharide capsular coats, making it difficult to create a broadly effective vaccine.
We are using a model of protective immunity to learn how the host immune system protects the host from repeated Kp infection. Based on preliminary data indicating that non-capsular antigens can elicit immunity to Kp that is lost in the absence of T cells, we are dissecting the role of T cells in our model of protective immunity. A variety of mouse lines with defects in select T cell subsets are being employed to define the specific features of the host immune response that protect from Kp infection. Ultimately, this work will help us understand host mechanisms that protect against Kp infection and how these responses can be activated by vaccination or immunotherapeutic strategies.
Immune recognition of Klebsiella pneumoniae O-antigen subtypes
Immunization is an attractive strategy to prevent Kp infections and reduce antibiotic use. The O-antigen polysaccharides are attractive vaccine targets as only four of the serogroups account for greater than 80% of infections. However, recent advances have led to the discovery of novel subtypes within the O-antigen serogroups. Currently, it is unknown what, if any, cross-protection exists between subtypes of serogroups.
This project aims to determine the relative pathogenic fitness, immunogenicity, functional antibody response and cross-protection (or lack thereof) of distinct subtypes within the same Kp O-antigen serogroup to directly impact Kp vaccine design.